ABC SURGERY
Vasectomy Is…
Developed as a means of contraception in the early 20th century, and popular (500,000 procedures per year) since the 1950’s, vasectomy is a dependable method of birth control for men who think they will never want any or any more children. It is a simple 15 minute procedure performed in a doctor’s office or clinic with a local anesthetic. The objective is to prevent sperm from entering the semen, 95% of which is support fluid made by glands called the prostate and seminal vesicles, located in the pelvis behind and beneath the bladder (anatomy diagrams).
Before Vasectomy
Sperm are made in the testes. From each testis, sperm move through a long curled-up tube behind the testis (the epididymis) wherein they become mature. From there, they swim up a foot-long tube (the vas) which guides them up to the channel (urethra) through which men urinate and ejaculate. Just before entering the urethra, the left and right vas tubes are enlarged, and it is here, behind the bladder, where many sperm are stored between ejaculations. The easiest place to access the vas tubes is just above the testes where the vas tubes are just beneath the thin scrotal skin, easy to feel and very mobile.
Methods… (Our Preferences Are Below)
Anesthesia: An anesthetic solution can be injected with a tiny needle to numb the scrotal skin and the vas tubes, or a pressure spray applicator can be used to numb the skin and vas tubes without using any needles.
Access: During conventional vasectomy, one or two 1/2-inch scrotal incisions are made to gain access to the vas tubes. These incisions are later closed with sutures, which remain in place for about 5 days until they dissolve or are removed. During no-scalpel vasectomy (NSV), special instruments are used to perform the procedure through a single tiny access-opening on the front side of the scrotum. The 1/4-inch slit usually seals within hours, so no stitches are needed.
Blocking the vas tubes: Whichever technique of accessing the vas tubes is used, each vas (left & right) is divided about one inch above each testis, where it is just beneath the thin scrotal skin and very easy to reach. What is done with the ends of the divided vas tubes depends on the preference of the person performing the vasectomy. Some operators remove a piece of vas; others don’t. Some tie off one or both vas ends using permanent or absorbable sutures or the small clips used to stop bleeding blood vessels during other types of surgical procedures; others cauterize the ends so that they will seal by scarring. Still others simply place the divided ends out of alignment, by closing the vas sheath between the 2 ends with a suture or tiny clip so the ends won’t grow back together.
After Vasectomy…
The portions of the vas tubes within the pelvis still contain live sperm until they are all released. About 98% of men are sperm-free after 20 ejaculations and 12 weeks. In 5% of men, the semen may still contain some sperm (usually few in number and not active) for months, so it is important to have a semen sample checked (Post-Vasectomy Semen Analysis – PVSA) and to use other forms of birth control until it is confirmed by microscopic examination that the semen is sperm-free.
Sperm are still made by the testes but can no longer pass up through the vas tubes (anatomy diagrams). So the body adjusts: white blood cells ingest and digest the retained sperm, recycling the proteins back into the system for use in other body functions. Men usually notice:
-
- No change in the semen
- No change in sex drive
- No change in climax sensation
- No change in the testes or scrotum
- No change in erections
In fact, a recent study concluded that vasectomy positively impacts the sexual satisfaction of couples because there is less fear of a accidental pregnancy.
Risks…
Bleeding can occur during or after vasectomy by either method, but it is less common with NSV. If this occurs within the scrotum, drainage of a scrotal hematoma (blood clot) in a hospital operating room could be necessary. Smaller hematomas do not require surgical drainage, but tender swelling can last for 2 to 4 weeks. Both large and small hematomas are very rare. If the scrotal skin bleeds at the vasectomy access site, the scrotum can become discolored (black and blue) for about a week; this is more common than swelling, but painless.
Infection is also a rare complication.
Delayed Lightheadedness (feinting) with bodily injury can occur hours after vasectomy even in men who feel great when they leave the office. If a man is driving when this occurs, he could injure himself or others. If he is standing, he could fall and injure himself. We offer all patients a soft drink with caffeine and sugar to decrease the likelihood of this occurring, and we strongly recommend that men come and leave with a driver. Although we have never had a patient sustain an injury from this, delayed feinting and bodily injury should be considered a risk because it has occurred in other practices.
Sperm granuloma is a pea-sized (sometimes tender) lump on the vas tube at the vasectomy site, almost never requiring treatment. Some consider sperm granulomas beneficial, as they may increase the likelihood of success with vasectomy reversal. Periodic tenderness usually responds to an anti-inflammatory medication like ibuprofen, but over the past 20 years and 40,000 vasectomies, 5-10 men been so troubled by chronic tenderness that they chose to undergo removal of the lump, an office procedure performed under local anesthesia similar to the original vasectomy.
Congestion, tender buildup of sperm and white blood cells upstream from or at the vasectomy site, can occur anytime after vasectomy, but usually goes away with use of an anti-inflammatory drug such as aspirin or ibuprofen. About one in 2000 patients will experience chronic post-vasectomy discomfort (PVPS or Post-Vasectomy Pain Syndrome) severe enough that he will seek vasectomy reversal or neurolysis (division of the sensory nerves coming from the testes). A larger percentage (the medical literature says 1-15%) may have milder forms of chronic pain that can affect quality of life but not severely enough to seek surgical therapy.
Re-canalization is the development of a channel for sperm flow between the two cut ends of the vas. If this happens during the healing process (early), the semen never becomes sperm-free until the vasectomy is repeated. If re-canalization happens late (months or years after a man’s semen has been examined and declared sperm-free), an unplanned pregnancy could result; but the odds of this occurring is far less after vasectomy than the odds of pregnancy with any other form of birth control including birth control pills and tubal ligation (female sterilization). Failure rates of vasectomy vary with the technique used to obstruct sperm flow through the vas tubes. The early failure rate is about one in 2500 and the late failure rate is one in 3500 .
There are no proven long-term health risks (neither cancer nor cardiovascular disease) associated with vasectomy.
The risks of NOT having a vasectomy are all borne by the partners of men who choose to avoid vasectomy. And they are considerable!
Limitations of Vasectomy…
-
- Not 100% reversible *
- Must use other forms of birth-control until sperm-free.
- Does not prevent transmission of sexually transmitted infections (STI’s).
Advantages Of Vasectomy…
-
- Low one-time expense
- More dependable than any other form of contraception including female sterilization.
- Eliminates risks associated with birth control pills or shots and the IUD.
- Vasectomy reversals are less costly and more successful than tubal ligation reversals
- No need for inconvenient and less dependable methods, so there are…
no more worries!!!!
* – Since reversal attempts often do not lead to pregnancy, vasectomy should be considered an irreversible form of contraception. Statistics show that men who undergo vasectomy in their 20’s are more likely to seek vasectomy reversal than men who have vasectomies later in life. In fact, men in their 20’s and with fewer than 2 children should read our Special Message for young men. Before choosing vasectomy, couples, especially couples in their 20’s with fewer than 3 children, should consider all other forms of reversible contraception including birth control pills, shots, patches, and implants ; the IUD (intrauterine device); and barrier methods such as the condom and diaphragm. A nice review of these options is in the Planned Parenthood website. Couples using barrier methods should also be aware that, for those occasions when they are just unintended, EC (emergency contraception, or the “morning after pill”) is readily available at most women’s health services sites such as private primary care and gynecology offices and Planned Parenthood clinics. EC is effective at preventing pregnancy for up to 72 hours (perhaps longer) after the “careless” encounter (visit www.not-2-late.com for a list of EC providers in your area).
Men should not proceed with vasectomy if they feel they are being pressured to do so, if their private lives are temporarily unstable due to marital discord, or if they have not considered all reversible alternatives. For many stable men, circumstances change, and all men, especially younger men, should consider sperm storage as insurance against regret over vasectomy in the event of a major life change. If you have never caused a pregnancy, how do we know that you even need a vasectomy … or what we should expect if you ever opt for vasectomy reversal? Please see our Special Message for Men Who Have Never Caused a Pregnancy.
The Technique Of Dr. Hussain:
No-Scalpel … And No-Needle!
See a vasectomy procedure in video in YouTube
Dr. Hussain use the no-scalpel technique as shown in the YouTube video provided above, exposing each vas in turn through a tiny opening in the front scrotal wall under local anesthesia. Since the opening is so small, it is easy to apply anesthesia without the use of needles. A spray applicator (MadaJet®) delivers a stream of anesthetic so fine that it penetrates the skin and diffuses to a depth of about 3/16 of an inch, enough to surround and anesthetize each vas tube in turn as it is lifted into position beneath the skin. Most, about 99%, of patients require no more anesthetic than this for completion of the procedure itself without pain. Some, about 1%, of patients do require injection of a little more anesthetic, but since the skin and vas are already partially numb, injection of more anesthetic with a fine needle rarely causes more than the slightest sensation. The tiny opening in the dime-sized area of numb skin is made with a pointy hemostat: one tip makes a pinpoint opening, then the two tips are used to spread and enlarge the opening to about 1/4 of an inch. Since blood vessels in the skin are spread apart rather than cut, bleeding is less than when a scalpel is used, no stitches are required, and the opening is usually sealed closed (often barely visible) by the next day.
Once each vas tube is lifted through the small skin opening, it is divided under direct vision with fine surgical scissors. Nothing is removed; the ends of the divided vas are placed out of alignment and kept from rejoining by applying a tiny clip to the sheath surrounding the vas so that one end stays inside the sheath, the other outside. While extremely effective (failure rate less than 1 in 2000), the technique provides for easier reversal (less scarring than when sutures are used) in men who choose reversal later in life. Procedure time is about 15 minutes. Most men say it hurts less than having a blood sample drawn. Many have called it painless. (In an e-mail, one patient recounted his experience step-by-step here.) A scrotal support (jockstrap) is applied and should be worn overnight and reapplied, after a next-morning shower, when up and around for the next 2 days. Ice-packs are not necessary. Men are advised to recline on the evening of the vasectomy, light activity the next day, sex and full activity 2 days after the vasectomy. After vasectomy about half of men will take non-prescription pain pills (Tylenol or ibuprofen), often just to prevent expected discomfort; the other half don’t take any pain pills. About 1 in 1000 men will have enough discomfort to request a prescription pain medication. Semen samples can be brought or mailed (we provide the mailers) to the office twelve (12) weeks after the procedure to see if all stored sperm have been passed. Ninety-eight percent of men are sperm-free after 12 weeks and 20 ejaculations, some sooner, and a few men will not be sperm-free for 5 or 6 months. Evaluation of semen samples is included in the price. A copy of our vasectomy instructions and consent is available below and here as a PDF file.
Instructions before Vasectomy
-
- If your partner has already had a tubal ligation (female sterilization), of if she is pregnant now and may have a tubal ligation during a Ceasarean delivery, please read this Special Message.
- Understand the Alternatives to Vasectomy so that you are confident in your choice.
- Understand the “Instructions Following Vasectomy” below so that you know what to expect.
- Please shave the underside of the penis and the front wall of the scrotum, preferably before the day of the procedure. A bit of alcohol is used to clean the skin before use of the MadaJet® and it can sting slightly right after a fresh shave if the skin is chafed.
- Use no powder or deodorant in the genital area on the day of your procedure.
- Please wear a scrotal support (jock strap) or very tight underwear to the office on the day of your vasectomy.
- Be prepared to sign the operative consent sheet (part of the PDF file in the paragraph above) upon your arrival in the office.
- If possible, arrange to have someone drive you home. A flat tire or fender bender could lead to complications, and some men who leave the office feeling great will experience delayed lightheadedness. If you must drive yourself, drive in the right-hand lane so that you can pull over if you begin to feel lightheaded.
- Plan to do nothing but recline at home (sofa or bed) on the afternoon and evening of the vasectomy.
- Do not take any aspirin-containing medication for five days before the procedure.
- If your insurance company or HMO requires authorization, be sure to bring it or call our office (813-536-1430) a day or two before your vasectomy to see whether we have received it.
- To save time on your procedure day, please watch the Online Counseling Video and complete our Online Registration Form.
- If you are taking TESTOSTERONE for “low T” please list it as one of your medications when you do the Online Registration and read the info HERE.
- Eat before your procedure, a normal breakfast or lunch. Nervous men who do not eat beforehand are more likely to become lightheaded during or after their vasectomies.
- Half of the $690 will be paid at the first visit ($345) and the second half on the day of the procedure. If you have insurance we can provide you with a form to submit to your insurance company. This may help you with your deductible and/or may help you get re-imbursed by your insurance carrier.
Instructions following Vasectomy
-
- Spend a quiet evening at home, reclining in bed or on the sofa. Minimize activity. Some men have no pain at all after vasectomy. Many have mild discomfort that does not require pain pills. Sometimes the discomfort is in the groins or abdomen. That’s because the testes originate in the abdomen in embryonic life and drag their nerve supply with them as they migrate into the scrotum. So any issue in the scrotal contents can be perceived as an abdomenal process.
- Avoid aspirin for 2 days after the vasectomy. You may take acetaminophen (Tylenol or generic) if you have any discomfort, as well as Ibuprofen (Motrin, Nuprin, Advil or generic) and naproxen (Aleve) , which are both pain medications and anti-inflammatory drugs. Pain beyond 3 days, especially if accompanied by some swelling of the vasectomy sites above the testes, may signify excessive inflammation and then ibuprofen and naproxen are better choices. Some men will have more discomfort or tenderness 3-5 days after the vasectomy than they do for the first few days after their vasectomies. That’s because the body goes through a series of steps in responding to the new arrangement, and sometimes the later steps are more noticable than the earlier steps. Usually no reason for concern.
- No need for ice packs, unless you really enjoy having ice on your scrotum.
- You may remove your tight undershorts or scrotal support and take a daily shower starting the morning after the procedure. Replace the tight underwear or scrotal support and wear it whenever you are up and around for the next 2 days, during sports for the next 7 days.
- On the day after the procedure, you may walk and drive as much as you like, but no sports, yard work, swimming, or heavy lifting over 30 pounds. If your job is sedentary (office work or supervisor), you may return to work.
- Two days after the procedure, you may return to more strenuous work and regular activities, including swimming, wearing your scrotal support. When pain is gone and tenderness is minimal, you may return to the gym or to running, but on the first day back, do half of your usual workout: half the weight, half the reps, half the speed, half the distance, etc. If pain does not return, you may do your regular workout the next day. You may also swim in fresh or salt water two days after the vasectomy.
- Sex: When you no longer have any pain or tenderness, you may ejaculate. I have always recommended waiting at least 7 days for any form of ejaculation (i.e sex/masturbation), and the American Urological Association Vasectomy Guidelines recommend that men wait a week. Sooner ejaculation could prolong discomfort. Blood in the semen within the first few months after the vasectomy occurs in some men, but it is no reason for concern.
- No follow-up visit is required. You will be given Dr. Hussain’s cell phone numbers and if you have undue discomfort or any concerns, you should text one of them anytime after your vasectomy.
- It is normal to have some discoloration of the skin (black and blue) around the puncture site a day or two after the vasectomy. Some men will develop considerable discoloration of the scrotum about 4 days after the vasectomy. Blood from the deep vasectomy site comes to the surface as a purplish-blue mark, gets darker and spreads out like an oil slick, then gradually dissipates.
- Some men (about one in 20) will develop swelling and discomfort on one side, sometimes on both sides, starting anytime from 3 days to 3 months following vasectomy. This usually represents an exaggerated form of the normal inflammatory response necessary for sperm resorption and recycling. It is effectively managed with a 5-7 day course of ibuprofen 600 mg 3 times per day.
- At least 14 weeks AND 20 ejaculations after your vasectomy (both time and activity are important), have your semen tested to be sure that it no longer contains sperm and that it is thereby safe to stop other forms of contraception.
- No ejaculation for at least one week after the procedure to allow the cut ends to seal and avoid channels from developing.
Fees
› Pricing & Consultation
At our practice, we believe in transparency and convenience when it comes to your care. Below are the details for our vasectomy consultation and procedure pricing.
› Consultation Only
If you would like to schedule a consultation to discuss the vasectomy procedure, the cost is $100.
During this visit, Dr. Macias will review your medical history, explain the procedure in detail, and answer any questions you may have.
› Vasectomy Procedure
The total cost for the complete vasectomy procedure, including testing and follow-up, is $690.
To make it easier for our patients, payment is divided into two parts:
- 50% deposit is due when scheduling the procedure.
- The remaining 50% is due on the day of the procedure.
› Insurance
We accept most major insurance plans. If you would like to use your insurance for the consultation or procedure, please let our team know in advance so we can verify your coverage and provide an accurate estimate of any out-of-pocket costs.
We strive to make every step of your experience as smooth and affordable as possible while maintaining the highest standards of care and professionalism.
Frequently Asked Questions About Vasectomy

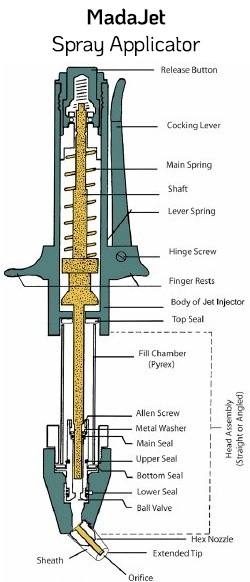
Traditionally, a local anesthetic has been injected into the skin and alongside each vas tube with a very fine needle, as small as diabetics use to inject themselves with insulin. One could feel a tiny poke in the skin, then a bit of a squeeze as the anesthetic was applied to each vas tube. However, most people do not like needles of any size … especially there!
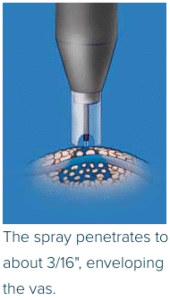
A MadaJet® is a spray applicator which delivers a fine stream of liquid anesthetic at a pressure great enough to penetrate the skin to a depth of about 3/16″, deep enough to envelop the vas tube held snugly beneath the skin. Each vas is positioned in turn beneath the very middle of the front scrotal wall and given two or three squirts. That numbs the skin and both vas tubes adequately for 99% of men. The other 1% (usually men who have thick skin or scarring due to prior surgical procedures in the area) will require a bit more anesthetic delivered with a fine needle, usually with no pain at all because of the partial anesthesia achieved with the MadaJet.
› Is this a “laser” vasectomy?
› How are the ends prevented from rejoining?


After the vas is divided, the upper (abdomenal) end is cauterized and allowed to slide back into its sheath, while the lower (testicular) end is held outside the sheath. A tiny hemoclip (the size of a grain of rice) is then used to close the empty portion of the sheath between the 2 ends. It would be like making a lengthwise opening in a wire’s insulation, reaching in and dividing the wire, lifting one cut end out through the insulation, then putting a clip on the empty portion of the insulation, thereby holding one end outside and one end inside, the insulation itself serving as a barrier between the two ends. Most hemoclips are made of titanium, a non-ferromagnetic metal used for many types of implanted medical devices such as dental implants, heart valves, and joint replacement.
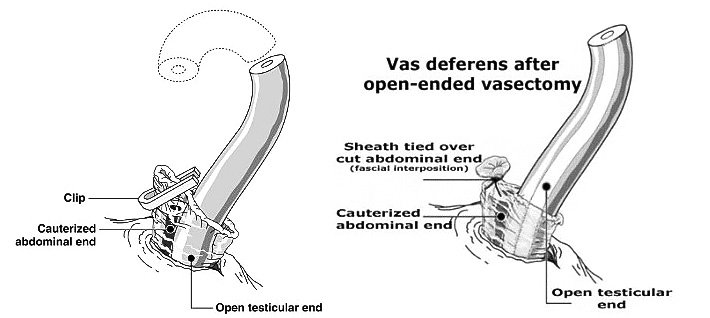
There have been no clip-related problems in the 38,000 or so men who have undergone vasectomy by Dr. Stein since he began using this method in 1990, and no reports of problems in the medical literature of which we are aware. Surgeons have used hemoclips for many years to occlude bleeding blood vessels during many operations in the abdomen and chest, sometimes over 50 clips in a single procedure. Hemoclips have been used by vasectomists for decades. In fact, during vasectomy reversal procedures, as many as 5 clips can be discovered on each side, clips of which the patient was unaware and which could not be felt by the surgeon before the reversal. Most hemoclips are made of medically inert titanium, the same metal used for dental implants, many artificial joints, and mechanical heart valves. Not ferromagnetic, titanium will not interfere with MRI studies and the small amounts used in hemoclips and dental implants do not set off metal detector alarms.
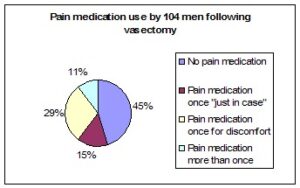
- 45% of men took no pain medication following their vasectomies, not even the Tylenol that was provided. They had so little discomfort that they saw no need to take anything.
- 15% of men took pain medication (the Tylenol that was provided or home supplies of ibuprofen) one time “just in case”, that is, as a precaution to prevent expected discomfort, not because they needed it.
- 29% of men took pain medication one time for discomfort, then did not need any additional doses.
- 11% of men took pain medication more than one time (two or three times), though at least 4 of these 11 men said that they had taken it more to prevent expected pain than because they were actually having discomfort.
- 0% of these men felt that they needed something stronger than Tylenol or ibuprofen, but we are asked for a prescription medication by about 1 in 500 men.
The previously common technique of removing a section of the vas tube (1/4 to 1/2 inch) and cauterizing the ends with a hand-held hot-wire cautery unit. Three patients (of about 1500) experienced early failure. That is, the vas tubes grew back together during the healing process, the men did not become sperm-free, and the vasectomies had to be repeated. Recognized early, the problem was corrected before an unintended pregnancy could occur. Since use of hemoclips to divert the vas ends out of alignment and only 7 anatomically normal men (of about 42,000 vasectomy cases, or one in 6000) have experienced early failure. Again, no pregnancies occurred because the men never became sperm-free and the vasectomies were successfully repeated without incident. Delayed failure, or late recanalization, presents as (1) a pregnancy after the semen has been confirmed to be sperm-free by microscopic examination, AND (2) documentation of a return of sperm to the semen by microscopic examination OR DNA documentation of paternity if the presumed father has no visible sperm in his semen (the veritable “one got through”). Delayed failure is also exceedingly rare. By contrast, the failure rate of birth control pills is 3% per year!
The expression “open-end” or “open-ended” refers to a vasectomy technique in which the lower (testicular) end of the vas is not occluded with a stitch, hemoclip, or electrocautery. The internet contains many web pages that laude the benefits of the open-end technique. The theory is that if the lower end is occluded, in effect “slamming the door” on the normal egress of sperm from below, there may be a sudden increase in pressure within the epididymis and the portion of the vas tube below (“upstream”) from the vasectomy site, potentially causing an increase in the level of inflammation normally required for the resorption of sperm. This exaggerated inflammatory response, so the theory goes, increases the likelihood of post-vasectomy discomfort and decreases the likelihood of reversal success, should the individual ever opt for vasectomy reversal in the future. After an open-ended vasectomy, a sperm granuloma may form at the vasectomy site with a transfer of the inflammatory sperm-resorption process to the vasectomy site, thereby sparing the upstream tubules (epididymis and vas) from this inflammation, decreasing the likelihood that they will become scarred and secondarily occluded, and enhancing the chances of reversal success.
› Are there any long-term health risks associated with vasectomy?
The February 17, 1993 issue of the Journal Of The American Medical Association contained 2 studies (by the same research group) that suggest that vasectomy was associated with a small increased risk of prostate cancer in their study groups (almost 30,000 patients in 1 study and almost 40,000 patients in the other study). Because the question was initially raised by 2 studies back in 1990, the World Health Organization convened a 1991 meeting of 23 international experts to review all research regarding vasectomy and prostate cancer. They concluded that there was no plausible biologic mechanism for a relationship between vasectomy and prostate cancer. Some medical researchers interpreted the small increased risk noted in the 1993 studies as a weak association that may be due to chance or bias. A systematic review of the medical literature in 1998 (Fertility & Sterility, 70: 191) further documented the lack of a significant relationship between vasectomy and prostate cancer. Additional convincing evidence of no relationship has been published in the Journal of Urology in June 1999 (161: 1848-1853), in the Journal of the American Medical Association in June 2002 (287:3110-3115), in the Journal of Urology in October 2002 (168: 1408-1411), and in Fertility and Sterility in November 2005 (84:1438-1443). A more recent study in 2014 raised the question once again, and once again, careful analysis of all available research data showed no association of vasectomy with prostate cancer. Studies as recent as 2016, show no increased risk of prostate cancer after vasectomy. The official position of the American Urological Association is that the association between vasectomy and prostate cancer risk is so weak that it need not even be discussed as part of routine pro-op counseling (see AUA Guidelines, pages 14-15). There are greater increases in the risk of prostate cancer (and mortality) associated with consuming milk/dairy products (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8255404/), meat (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8859108/#:~:text=Consumption%20of%20processed%20meat%20might,not%20with%20advanced%20prostate%20cancer) and alcohol (https://pubmed.ncbi.nlm.nih.gov/27842506/) or even having multiple sexual partners and not ejaculating often enough (https://pubmed.ncbi.nlm.nih.gov/30122473/).
The question of an association between vasectomy and subsequent cardiovascular disease was raised back in 1978 and 1980 by two studies which reported an increase in atherosclerosis (hardening of the arteries) in vasectomized laboratory monkeys. The last article listed above (Cancer and cardiovascular disease after vasectomy: an epidemiological database study. Fertility and Sterility 84:1438-1443, November 2005) provides an excellent bibliography of studies showing no association in humans as well as its authors’ own data comparing 24,773 vasectomized men with 159,480 non-vasectomized men as a control group. Their findings “strengthen the evidence that vasectomy is not followed by an increased risk of myocardial infarction [heart attack], coronary heart disease as a whole, or stroke. In particular, we add strong support to the evidence that there is no elevation of risk of cardiovascular disease in men after long periods after vasectomy.”
My office has copies of these and other research studies, available to any patient upon request.
Federal programs (Medicaid and Title10) that provide financial coverage or assistance for sterilization procedures require only that the candidate “is at least 21 years old and appears mentally competent“. There are no laws forbidding vasectomy for certain age groups, though individuals under 18 require parental consent for any elective surgery. We will not provide vasectomy for a childfree man under 21 years of age unless (1) there are profound extenuating circumstances such as a hereditary disease or obvious inability to care for a child, as might be the case in someone with a cognitive disability, or (2) he presents documentation of sperm storage. We have provided vasectomy for men younger than 21 who have had 2 or more children. Other vasectomy providers may follow a different or more restrictive set of guidelines, as is their prerogative.
Special Message for Young Men with Fewer than Two Children
If you are less than 30 years old and you have had fewer than 2 children, please consider the following points before having a vasectomy:
- You may regret it. Men who have vasectomies when they are in their 20’s, especially if they have had fewer than two children, may be the ones most likely to seek vasectomy reversal at a later date, often regretting their vasectomy decisions if their reversals are not successful.
- You may change. Many men who think they will never want children when they are in their early 20’s are delighted with fatherhood when they are in their 30’s. You may be totally convinced now that you will never want children, but people change and you may have a much different outlook 10 years from now.
- Women change. Similarly, women who have no desire for children when they are in their early 20’s may have a much stronger desire when they are in their 30’s and when many of their friends are having children of their own.
- Relationships end. Since more than 50% of American marriages end in divorce, you may not be with the same partner ten years from now and a new partner may have a much stronger desire for children than your present partner does. So just because your present partner claims that she will never want children, her tune may change 10 years from now, or she may not even be your partner 10 years from now.
- The philosophy of you and your partner with respect to abortion should be considered. If you are both not philosophically opposed to abortion, you have some back-up should other forms of contraception fail, and having a vasectomy now may not seem as critical to avoid an unintended pregnancy. But keep in mind that if she gets pregnant, the choice is hers.
- Vasectomy should be considered a permanent and non-reversible procedure because vasectomy reversals are not always successful. So before having a vasectomy, know all of the other options … HERE and HERE.
- Young men should consider Sperm Storage. The companies who provide the service will send what you need directly to your home, you can collect the semen specimens in the privacy of your home, and you can mail them back to the company in the storage container provided. Imagine meeting a prospective partner years after your vasectomy. You fall very much in love with her, but you know that she will someday want children. You can tell her, “I have had a vasectomy”, or you can say, “I have had a vasectomy, BUT I banked sperm for future use.” Now, which do you think will sound better to her? In her eyes, either you did a foolish thing years ago, or you made a responsible decision with good foresight. In one case, you may lose the girl; in the other case, you win her heart. So sperm storage can be a very smart thing, well worth the investment.
- Have you discussed your decision with your parents? If not, consider this: You’re an adult, yes, but they helped you get there. How would you feel if your son came home one day and said that he had had a vasectomy? That he had done something to limit his future potential (to be a father) and to limit your own potential (to be a grandfather). How would you feel, after nurturing and guiding him for over two decades, if he did something to profoundly influence his future, but did not have the respect or courtesy to just tell you about it beforehand? As with many decisions in life, change the question from, “Should I tell my parents?” to “What can I do that I will never regret?” Would you ever regret not telling them? Possibly, especially if they are hurt as I, as a parent, would be. Would you ever regret telling them? Probably not. Having a vasectomy is still your decision, but at least you granted them the respect of letting them render an opinion. And if they succeed in discouraging you, because they know you better than any doctor does, you may one day thank them. If they don’t succeed in discouraging you, they may split with you the cost of sperm storage and feel much better about your vasectomy in doing so.
All of this said, I recognize the fact that most of us know someone whose girlfriend said she could not get pregnant, or conveniently “forgot” to take her pills, or even poked pinholes in his condoms. And I recognize that our judgments can be impaired after a few drinks so that we are less inclined to cover up or pull out on time. Indeed some men perceive the risks of not getting a vasectomy to be greater than the risks of getting one. We must all be masters of our own destinies, and that is easier if we think through all of the implications, alternatives, and potential consequences of our decisions.
